In the booming fertility business, young women face unfavourable conditions and undergo multiple egg donations at the risk of their health.
It was a hot afternoon in October 2019, and 22-year-old Joan* had just been crying in a ward of a private hospital in Mokola, a neighbourhood of Ibadan in southwestern Nigeria.
Seven days earlier, she had started taking hormone injections to stimulate her ovaries into producing mature eggs, part of the process to get her body ready so that the doctors could extract them.
Joan felt a bit uncomfortable from the examination and had a few painful spots on her lower abdomen where she had been jabbed by the hormone injections. But her tears were not due to the invasive nature of the procedure. Rather it was the doctor’s demeanour, which she says was rude and condescending.
“When he came in to do the examination, I asked him if it was possible to get a female gynaecologist since a female one examined me during my initial visit. He flared up, said no female gynaecologist was on duty,” she recounts. “He proceeded to ask what was so special about my body, said he had seen plenty [of] vaginas before, even that of a beauty queen … and he even mentioned her name.”
Joan visited a clinic to get more information. “It felt like a win-win because I know how hard it can be for a woman to have children, so I took it as me doing a favour and still getting paid for it,” she says.
The screening process and eligibility procedures vary from one clinic to another. Joan describes what hers entailed: “They took my blood sample, had tests done for genotype, HIV, hepatitis, and they asked many questions about my health and medical history. Afterwards, I was told to come back during my period which is the beginning of my menstrual cycle.”
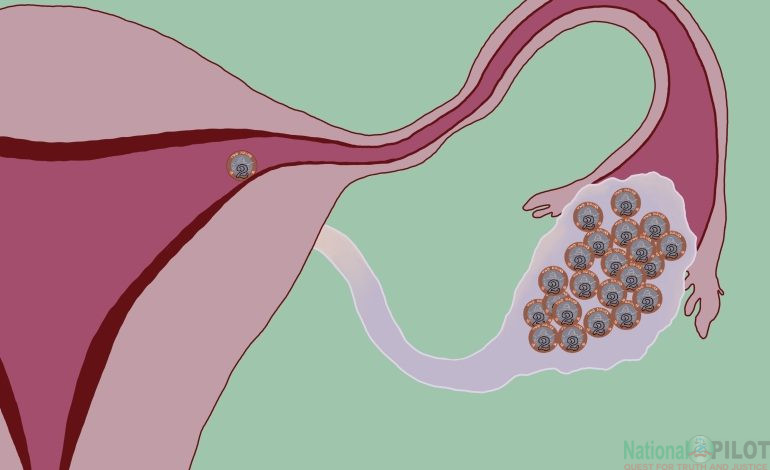
The process from beginning hormone injections to egg retrieval takes approximately 13 to 15 days, depending on the body’s response to the stimulating hormones.
Joan had to start taking the injections at home – self-injecting her lower abdomen just under the navel every day. After a week, she returned to the hospital to see how the eggs were growing.
“When I went to the clinic, they checked and said I had like seven eggs already, and that if I could do like five more days or six, that we could probably get like double the number, just to increase the odds.”
It was then that she had the unpleasant encounter with the doctor.
Despite already being halfway through the donation process, Joan walked home from the clinic, plagued by the headaches that began when she started taking the hormone injections, intending to quit the whole thing.
But she could not because she needed the money.
Nigeria’s unemployment rate of 33.3 percent in 2020 – a number that is steadily rising – plus its high inflation rate negatively affects the economic mobility of many citizens. Against this backdrop, the promise of money is a big incentive for many young people to do things they would not ordinarily consider.
It is the primary reason Esther*, a 26-year-old baker who sells cakes and pastries from her home in Lagos, has donated her eggs six times since February 2020, even though experts like the American Society for Reproductive Medicine recommend that women should only donate their eggs six times in a lifetime.
But with the government-mandated minimum wage in Nigeria at 30,000 naira ($73) per month, and even the least well-paid egg donation paying more than double that per round, many are willing to accept the potential health risks.
Esther’s first donation was done through an agency and she was paid 100,000 naira ($243). Such agencies actively recruit and screen potential donors for the private clinics they are affiliated with, and if certified eligible, set donors up for egg stimulation injections and subsequent retrieval in the clinic. Some agencies – like the one Esther went to – also pay women extra for referring new donors.
Esther did all the tests the clinic requested, and was told to come back when she was menstruating. Concerned about donating her eggs again so soon, she delayed. But they called again so she went back two months after her first donation; the clinic even helped pay for her transport with an extra 1,500 naira ($3.66) travel allowance for each day she went in.
“The nurse who attended to me had so many rules – drink water, don’t use perfume, don’t shower in the midday, don’t have sex – but I know she was just doing her job and there were so many of us. She was so cranky and would not even answer questions,” she says.
The procedure sometimes can be painful … But it’s bearable, especially with the money.
“The first donation I had at the clinic in May was very painful,” she remembers. “Every day, I had to go to the hospital for an injection on my thigh. After the first three days, my stomach felt very swollen, and I lost my appetite. I could barely walk yet I had to go for the injections daily. I think it was the stress of all that movement, but it was so hard. The money they offered was 120,000 naira [$292] which was way more than the 100,000 [$243] the agency paid, so I pushed through.”
All the payments were made through bank transfers and she received the funds the very same day, she says.
But there were side effects. “After the [second of her six] donations, I had to go back for treatment because I was in severe pain, and I even had to pay for it [myself] … My belly was cramping so bad. I was admitted, given drips and a couple of injections.” This was a result of the amount of hormones she had injected and the fact that she had left little time between donations.
When asked if she has concerns about how it may affect her health in the future, she says, “Well, the procedure sometimes can be painful, and I often have painful severe cramps with heavy flow on the next period.
“But it’s bearable, especially with the money,” she laughs.
After a minute’s silence, she continues, “They didn’t mention any long-term effects – not at the clinic or agency but I’ve also read about it, there’s nothing to worry about. At times, I worry about the possibility of exhausting my eggs, but I read somewhere that we have so much so that’s near impossible. Also, I don’t have plans of ever giving birth so there’s that.”
The egg retrieval process
The procedure for egg retrieval is usually completed within 30 minutes with the patient under sedation. A needle is passed through the posterior vaginal wall into the ovaries under ultrasound guidance. The mature follicles are then aspirated via the needle into test tubes. This process is repeated for the second ovary. The patient is given analgesics and antibiotics afterwards and is put on bed rest to allow the sedation to wear off.
Abdulgafar Abiodun Jimoh, a professor and consultant in gynaecology and obstetrics at the University of Ilorin Teaching Hospital, says the most common immediate effect is pain, with donors experiencing varying degrees of it.
However, there is more. “There’s the possibility of hyperstimulation syndrome which may be mild, moderate or severe,” he explains.
This is a complication where the excess hormones cause the ovaries to grow large and the blood vessels surrounding them to leak fluid which causes swelling. Depending on the severity, this excess fluid can move into the abdomen, lungs, and chest regions. It manifests as severe discomfort, abdominal distension and pain, breathing difficulties, liver and kidney dysfunction and coagulation problems.
“In severe cases, it can be problematic, even fatal. Although it is exceedingly rare, it has been reported. They may need surgery, you may have to drain, they can go into shock, they can experience kidney shutdown and the likes too,” the professor explains.
“Apart from that, there’s a theoretical small chance of getting an infection during the procedure, especially as you’re putting your needle directly into the peritoneum – that’s where the ovaries are. The bladder and intestines are all within the vicinity of where the eggs are. If you mistakenly go into the intestine and come out, you’ve already picked some bacteria so transfers can happen. These are the potential risks.
“However, these risks are relatively uncommon, especially if good protocols and best practices are followed.”
Jimoh says although egg donation “is fraught with problems”, these problems are “largely mild, not devastating, not life-threatening enough to discourage people from doing it – often repeatedly”.
Government regulations
It is estimated that at least one in four Nigerian couples may require assisted reproductive technology (ART) such as IVF. However, laws and policies are not being developed fast enough to meet the demands of this growing industry, experts say.
A bill for the establishment of a Nigerian Assisted Reproduction Authority to regulate this practice was presented before the National Assembly and read for the second time on May 2, 2012. It was referred to the Committees on Health and Justice but has not yet been passed into law.
Professor Jimoh points out that Nigeria is not alone in being slow to implement laws in this area. “It is only within the last 10 years that the UK itself has been able to come up with a regulation that says you’re not supposed to get paid for it [egg donation]. In the EU, the legislation is still far in between each of the countries. In Nigeria, we certainly do not have legislation yet but we have acts of parliament in place meant to form a law that governs assisted reproduction in this country.”
In 2014, the National Health Act was enacted. It is currently the only legal framework governing egg donation in Nigeria. Section 53 of the Act criminalises the exchange of human tissue and blood products for money, even allowing for a fine and/or up to a year’s imprisonment for those convicted. But the people spoken to for this story were unaware the law existed and unsure how it would apply to egg donation.
Speaking about the lack of actionable laws, Amarachi Nickabugu, a Nigerian lawyer, says, “There is a need for laws to protect the donor, recipient, and caregiver as well, one that defines who can be involved in the techniques and the guidelines for practice as well as stipulate punishments for those who violate the rules of the practice. Because the odds favour eggs from young women, most donors are young women, often undergraduates, and they do this from a vulnerable, powerless, and penniless place. It is financially coercive, and it is important for there to be legal protection against exploitation for them.”


Explaining a loophole in the Health Act, Nickabugu says, “The National Health Act prohibits trading in human tissues. However, it does not explicitly outlaw egg donations. So, the question is, are the egg donors ‘donating’ their eggs or ‘selling’ them?”
Clinics could, in theory, describe payments as monetary compensation for the costs accrued during egg donation rather than as payments for the eggs themselves.
The other side
Fertility medicine may be a fast-growing sub-sector of the healthcare system, but high costs and the fact that it is not covered by the National Health Insurance Scheme (NHIS) mean it is out of reach for many Nigerians.
A consultation with a fertility specialist can cost in the range of 50,000 naira ($121) to 110,000 naira ($268). Intrauterine insemination (IUI) has an estimated cost of 320,000 naira ($780), and a single-cycle IVF treatment with donor eggs costs 252,000 naira ($614) excluding drugs, legal and scheduling fees.
Thirty-seven-year-old Adefunke* has had two unsuccessful rounds of IVF using eggs from donors like Joan and Esther. But she is still hoping for a miracle.
After being married for 14 years without conceiving a child, her husband has now taken a second wife.

“I’ve never been in contact with any of my egg donors,” she says. “They were all anonymous donations … We were required to fill a form stipulating the conditions we want – things like tribe, complexion, genotype and the likes. Actually, there were a lot of forms …
“We also had to do lots of tests. The doctors match us for genotype, blood group and other medical modalities. For my first session, it was my husband’s sperm we used. But not for the second.”
The experience of donating? Never again … It’s one of those things I try to suppress and put at the back of my mind like it never happened.
Adefunke went through the process at a private clinic that she and her husband were referred to by their family doctor. Following consultations and tests, the clinic matched them with a donor. Adefunke says she paid 2.2 million naira ($5,362) for the first attempt and 2.6 million naira ($6,337) for the second.
Reflecting on the anonymous egg donors, she continues, “I don’t know what they go through, but I know it can’t be easy on them. But I am grateful to them for doing it, even though I know their major incentive is the money.”
This is what donors like Joan take comfort in. “Whatever happens, I just hope one or two mothers are out there with their babies and happy,” she says.
But as in Adefunke’s case, IVF often has a low rate of success, meaning many people will be left poor and childless. “We often have about a quarter of successful cases, about 25-30 percent. In some of the unsuccessful cases, they might come back,” says Professor Jimoh.
Joan went back to the clinic five days after her bad encounter with the doctor and was seen by a different one. After a quick examination, she was told to return the next day for the egg retrieval.
The procedure did not take long, and for Joan, it was not a painful one.
A few hours after she got home that day, she got an alert telling her 100,000 naira ($243) had been deposited into her bank account.
While she is glad at the opportunity to help women conceive, Joan says it is not something she would consider going through again.
“The experience of donating? Never again … It’s one of those things I try to suppress and put at the back of my mind like it never happened.”
But she says she understands why it is a booming industry.
“You should have seen the people at the hospital, people that were desperate to see the doctors for treatment,” she reflects. “If I was in a position like that, I’ll also pay as much money as I can.”
*Names have been changed to protect the privacy of the egg donors and recipients.
Source: Al Jazeera





